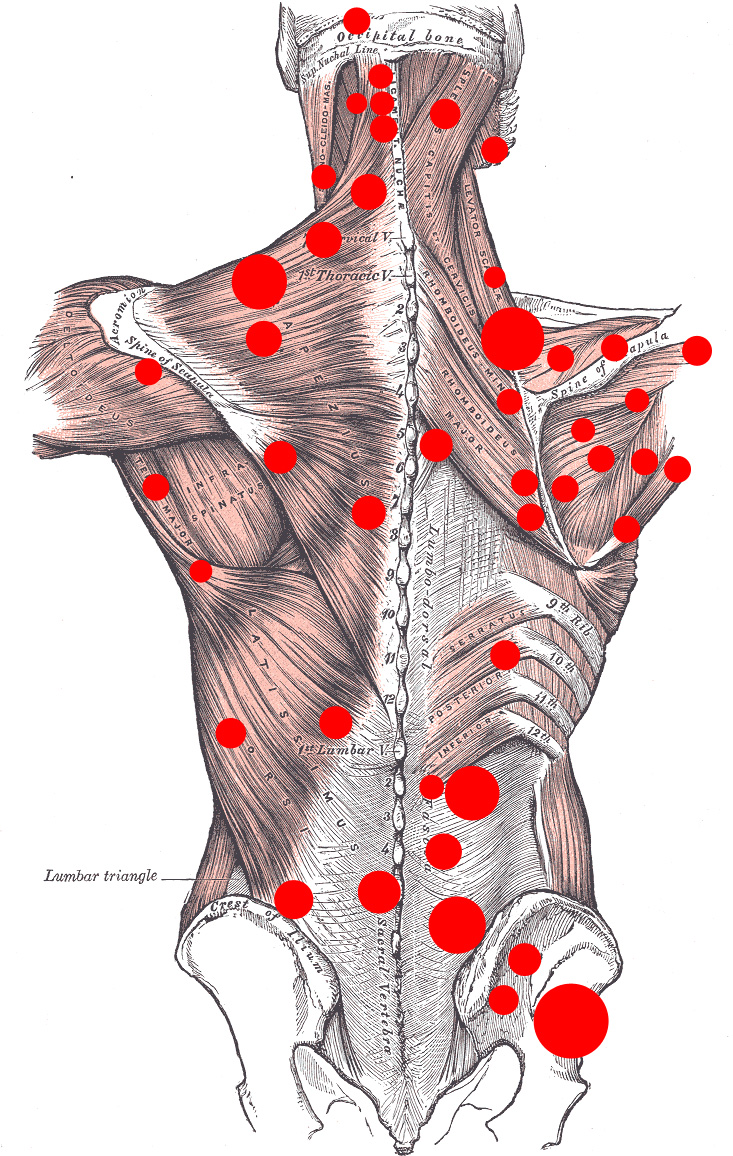
 Myofascial pain syndrome is a chronic musculoskeletal pain disorder that can involve either a single muscle or a muscle group. It refers to pain and inflammation in the body’s soft tissues. Myofascial pain is a chronic condition that affects the fascia (connective tissue that covers the muscles).
Myofascial pain syndrome is a chronic musculoskeletal pain disorder that can involve either a single muscle or a muscle group. It refers to pain and inflammation in the body’s soft tissues. Myofascial pain is a chronic condition that affects the fascia (connective tissue that covers the muscles).
The pain associated with this condition can range from burning, stabbing, aching sensations to include a combination of these symptoms. With myofascial pain syndrome, excessive strain on a particular muscle, muscle group, ligament or tendon can prompt the development of a “trigger point” that, in turn, causes pain.
Where a person experiences the pain may not be where the myofascial pain generator is located. This is known as referred pain. Myofascial pain symptoms usually involve muscle pain with specific “trigger” points which can be made worse with activity.
What causes myofascial pain & what are the symptoms?
Myofascial pain typically occurs after a muscle has been contracted repetitively. This can be caused by repetitive motions, injury to an intervertebral disc, or lack of activity (such as a broken leg).
The main symptom of myofascial pain is ongoing muscle pain, in areas such as the low back, neck, shoulders, and chest. These symptoms may include a muscle that is sensitive or tender when touched, or a pain that feels aching, burning, stinging, or stabbing and does not lessen in intensity. Another symptom is reduced range of motion in the affected area and a feeling of weakness in the affected muscle.
How is myofascial pain diagnosed?
Trigger points can be identified by pain produced upon digital palpation (applying pressure with one to three fingers and the thumb). In the diagnosis of myofascial pain syndrome, four types of trigger points can be distinguished:
- An active trigger point is an area of extreme tenderness that usually lies within the skeletal muscle and which is associated with a local or regional pain.
- A latent trigger point is a dormant (inactive) area that has the potential to act like a trigger point.
- A secondary trigger point is a highly irritable spot in a muscle that can become active due to a trigger point and muscular overload in another muscle.
- A satellite myofascial point is a highly irritable spot in a muscle that becomes inactive because the muscle is in the region of another trigger pain.
How is myofascial pain treated?
Treatments may include any of the following:
- Massage Therapy
- Physiotherapy
- Lifestyle changes -adjusting your workstation, improving posture, avoiding muscle tension
- IMS | Trigger point dry needling
- Transcutaneous electrical nerve stimulation | TENS
- Laser
- Ultrasound
Often a combination of physical therapy, trigger point dry needling and massage are needed in chronic cases. Please talk with one of our health care practitioners to discuss myofascial pain syndrome.

 When Tracy Tarnowski was diagnosed with breast cancer, she opted to have a double-mastectomy, even though her malignancy was confined to only one breast. But the tumour was widespread and aggressive – and she wasn’t about to take any chances.
When Tracy Tarnowski was diagnosed with breast cancer, she opted to have a double-mastectomy, even though her malignancy was confined to only one breast. But the tumour was widespread and aggressive – and she wasn’t about to take any chances. Scientists have just found a way to use DNA to send massive amounts of data between cells, which means we soon may be able to give our cells incredibly complicated instructions.
Scientists have just found a way to use DNA to send massive amounts of data between cells, which means we soon may be able to give our cells incredibly complicated instructions. It’s been seven years since the Supreme Court of Canada struck down Quebec’s ban on using private insurance for “medically necessary” services covered by medicare.
It’s been seven years since the Supreme Court of Canada struck down Quebec’s ban on using private insurance for “medically necessary” services covered by medicare. In Autumn, we observe nature withdrawing inward. We see leaves wither on the branch as the trees gather energy inward and down to the deep center and roots to protect and guard vitality, like a precious secret, throughout the winter months.
In Autumn, we observe nature withdrawing inward. We see leaves wither on the branch as the trees gather energy inward and down to the deep center and roots to protect and guard vitality, like a precious secret, throughout the winter months. The first question you need to ask is; is a half marathon a good idea for every marathoner?
The first question you need to ask is; is a half marathon a good idea for every marathoner? Degenerative disc disease is one of the most common causes of low back pain.
Degenerative disc disease is one of the most common causes of low back pain.
 Orthotics
Orthotics